More Than a General Agent, We’re Your Strategic Partner.
Our Approach to Broker Solutions & Support
Serving as a unique, single-source liaison Between 450+ independent insurance Brokers and the premier Central Pennsylvania healthcare carriers, AIA, Alera Group’s broker solutions division is fundamentally distinctive to other general agencies. We understand that it is now important more than ever to protect your client relationship. By selling quality group employee benefit products; we strengthen your relationships, while adding more revenue to your bottom line.
With over 50 highly-qualified professionals, we ensure that the strategic, technical, and operational support we provide to our broker partners represents the full spectrum of services such as relevant human resource, consulting, technology and employee benefits expertise. We are confident that we can serve and support our brokers with competitive strategies and innovative strategies.
We believe:
- Communication, care, and attention to detail is critical for your success
- Instant, competitive pricing analysis for all premier Pennsylvania healthcare carriers ensures you will reach your client goals
- Innovative self-service tools set you apart from other brokers
Our Expertise and Capabilities
AIA, Alera Group has deep, proven expertise to help separate you from your competition. Here a just some of our expert service and solutions include (Click the + button on any service below for further explanation):
The Power of Detail—Analytics  Our Health Care & Benefit Analytics team maintains the primary responsibility for the development of actuarial-based financial deliverables for the large group market. Our analytical portfolio serves as the foundation to the most sophisticated education, expertise and collaboration to differentiate our Broker Partners from their competition!
Our Health Care & Benefit Analytics team maintains the primary responsibility for the development of actuarial-based financial deliverables for the large group market. Our analytical portfolio serves as the foundation to the most sophisticated education, expertise and collaboration to differentiate our Broker Partners from their competition!
Our Approach
Rather than the typical annual-renewal approach deployed by most brokers/consultants, AIA, Alera Group broker partners can access our expert underwriting & analytical team to assist them in creating multi-year strategic health care plan designs, employee health & well-being plans, and employee communications. This allows you to focus on helping your clients achieve their financial objectives and strategic goals, avoiding the annual crisis situation many companies face at renewal time. Your clients will praise you!
We Know Your Data
Your client’s historical medical, pharmaceutical, and disability claims trends are a treasure trove of information. Your AIA, Alera Group team has developed sophisticated analytical models that enable us to give you a comprehensive view of your client’s unique situation. From that information, we can recommend alternative approaches, along with the cost and benefit of each scenario. With our analysis and your data, you will feel confident that your clients are making the best decision possible.
Positive Financial Impact
We translate the health carrier data into our proprietary analytical models, extracting all useful information and consulting observations that provide the root connections to the real problems your client is or could be facing…and the solutions! The process of better thinking applied to detailed data creates better outcomes for both your client and their employees. Here is a sampling of better outcomes we produce:
- Accurately forecasted carrier renewals and self-funded budgets well in advance of typical renewal planning schedules
- Successfully negotiated fully-insured and reinsurance renewals based on carrier-recognized underwriting observations contained in our proprietary reports
- Accurately forecasted self-funded claims impacts from plan design changes
- Well-founded decisions to move from fully-insured to self-funded and vice versa
- Appropriate cost-sharing strategies between employer and employee
- Cost-reducing pharmaceutical carve-out arrangements
- Strategies for cost reduction
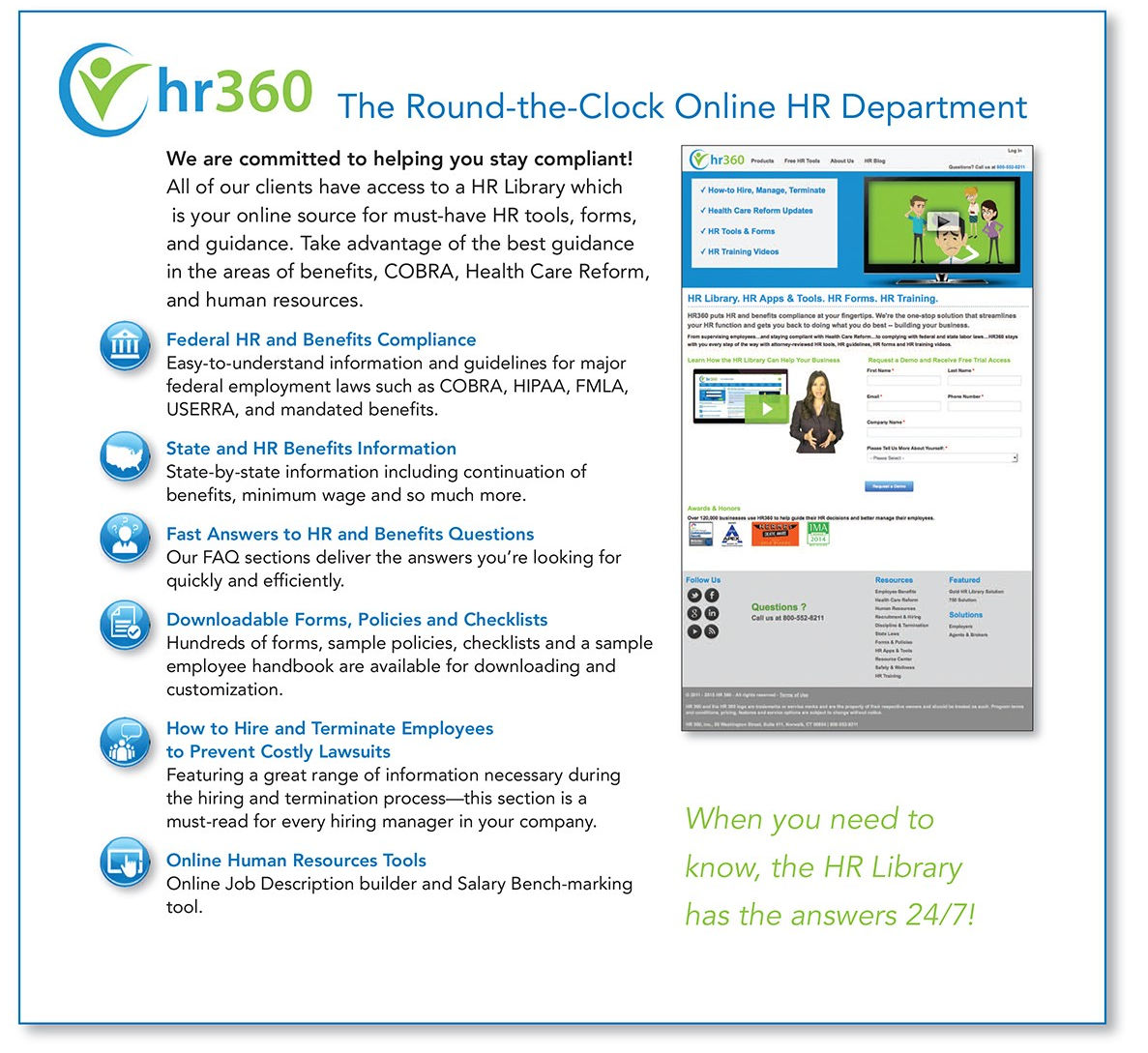
The Power of Expertise—Compliance & HR Advantage
 In the current landscape of employee benefits, staying compliant with the latest laws and regulations can be overwhelming. Our compliance team is a national Alera center of excellence and provides the latest information, legal alerts, and expert analysis so you can navigate the complexities of healthcare reform and help your clients avoid unnecessary risk and fines from non-compliance. In addition, our HR portal provides a one stop solution for attorney reviewed HR news, tools, forms, and training!
In the current landscape of employee benefits, staying compliant with the latest laws and regulations can be overwhelming. Our compliance team is a national Alera center of excellence and provides the latest information, legal alerts, and expert analysis so you can navigate the complexities of healthcare reform and help your clients avoid unnecessary risk and fines from non-compliance. In addition, our HR portal provides a one stop solution for attorney reviewed HR news, tools, forms, and training!
Education
- Live Q&A assistance-dedicated broker email and phone services
- Regulatory, HR, and compliance webinar series-available to brokers and their clients
- Fully customizable broker newsletters and compliance corner alerts
- Customizable monthly newsletter-Benefit Bullets
- PPACA client presentations
- Face-to-face or webinar presentations available to broker clients
- Regulatory and model notices
Expertise
The power of unmatched legislative and HR consulting is available to you through our compliance team. Strengthen your client services portfolio and differentiate your agency from the competition. We offer:
- Healthcare reform consulting services
- PPACA risk mitigation
- Scenario modeling
- HR risk management
- Basic PPACA diagnostic analysis, including:
- Group size determination
- Individual subsidy eligibility
- Pay or play analysis
- Transition relief analysis
Administration*
AIA, Alera Group broker solutions can conduct a review of your client’s benefits policies and practices in the following areas:
|
|
| *Additional fees may apply for some services. | |
The Power of Efficiency—Instant Quoting & Proposals
 Leveraging knowledge and technology provides a powerful outcome! As an AIA, Alera Group broker partner, you have exclusive access to our industry leading online quoting and proposal system—intuitive logic to produce rates and plan design comparisons instantaneously! Create a Contribution Summary with ACA regulatory provision logic already included to ensure that your clients receive fast and accurate proposals based on their unique demographics.
Leveraging knowledge and technology provides a powerful outcome! As an AIA, Alera Group broker partner, you have exclusive access to our industry leading online quoting and proposal system—intuitive logic to produce rates and plan design comparisons instantaneously! Create a Contribution Summary with ACA regulatory provision logic already included to ensure that your clients receive fast and accurate proposals based on their unique demographics.
Industry Leading Quoting and Proposal Solution
- The moment your census is uploaded, you will instantly have rates across all carriers to help you and your client make informed decisions.
- Rates are categorized by quarterly effective dates.
- Zip code database is integrated to ensure correct zone.
- Individual age is calculated off effective date and rates are populated instantly.
- ACA Dependent Counting per family unit is automatically applied.
- Plans can be conveniently grouped by carrier or in premium order.
- A proposal is created exclusively for your client, complete with ability to manipulate contribution and funding strategies.
- Review carrier rates by group total or by each individual listed on census.
- A change or deletion instantly reveals the impact to rates, contribution strategies and funding arrangements.
The Power of Connectivity—Benefits Administration & Technology
 Gain access to world-class benefit administration and technology service providers through the AIA, Alera Group established relationships. We help you with the latest and best solutions to reduce the benefits administration cost and improve efficiency for your clients, something paramount to rising above your competition.
Gain access to world-class benefit administration and technology service providers through the AIA, Alera Group established relationships. We help you with the latest and best solutions to reduce the benefits administration cost and improve efficiency for your clients, something paramount to rising above your competition.
Benefits Administration Services
We provide exclusive access to superior benefits administration platforms designed to offer HR ease and effectiveness to your clients. The benefits administration portfolio exclusively available to our broker partners includes our:
- Stand-alone benefits administration with employee self-service
- Total compensation statements
- New hire onboarding and orientation
- ACA tracking/reporting
- Employee lifecycle management
- Audit current HR technologies and workflows, identify efficiencies and gaps (100+)
- Assist with selecting the right HR technology to meet customer needs (100+)
To implement this platform, your AIA, Alera Group team meets with your client’s HR and Benefits team to analyze their client-specific requirements. Once identified, we work together with you and your client to design and construct processes and systems, perform testing, train the HR staff and users in the administration of the systems, and acceptance to ensure a smooth implementation.
Additional Technology Resources
We also offer additional technology resources important to the administration and reporting of benefit programs. Through specific strategic vendor alliances, sophisticated technology, and effective tools our broker partners are able to be more responsive, informed, and competitive. Some of these technology resources include:
- Payroll vendors
- ACA reporting (Stand Alone Available)
- Third-party administrators (HRA, HSA, COBRA)
- Email encryption and archiving solutions
- Agency Management System
The Power of Alliances—Health Advocacy & Well-being ![]() Gain access to world-class service providers through direct relationships we developed on your behalf. Offering cost-effective, superior solutions in a variety of critical areas that maximize employer dollar value while enhancing employee satisfaction and appreciation. These are available to our broker partners at significantly lower costs than those available outside your partnership with AIA, Alera Group.
Gain access to world-class service providers through direct relationships we developed on your behalf. Offering cost-effective, superior solutions in a variety of critical areas that maximize employer dollar value while enhancing employee satisfaction and appreciation. These are available to our broker partners at significantly lower costs than those available outside your partnership with AIA, Alera Group.
Health Advocacy & Well-being Solutions
As the landscape of the healthcare industry changes, managing (lowering) healthcare costs and improving employee health have become critical issues for employers. Wellness initiatives have become exceedingly popular among employers, and while there are numerous solutions to choose from, many have not demonstrated proven results.
As an AIA, Alera Group broker partner you gain exclusive access to our DiscoverHealth® unit, distinctly created to help “bend the healthcare cost curve” for employers and improve the well-being of their employees. DiscoverHealth® offers an encompassing portfolio of services that embrace five essential areas of employee well-being and provides a cost-effective strategy for improving employee health. We have performed due diligence on each portfolio program, and members of DiscoverHealth® have been certified by the Intel/GE Care Innovations Validation Institute which designates our ability to effectively evaluate wellness and well-being solutions available in the marketplace to discern programs with realistic outcomes and results.
Broker partners can confidently offer their clients a variety of population health management and well-being solutions that are aimed at improving the health of workforce and lowering healthcare costs including:
- Targeted nurse coaching-Individual health coaching based on assessed health risks
- Care Gap Reduction-Medical/prescription claims data mining
- Metabolic Syndrome Risk Factor Reduction-Solutions to provide individuals with ongoing support to address key risk factors contributing to Metabolic Syndrome
- Health Screenings and Patented Disease Risk Questionnaire-Screenings combined with a multi-dimensional tool to predict risk of onset and progression related to multiple chronic diseases
- Health Advocacy & Pricing Transparency-Services to improve consumerism, giving employees resources for cost transparency, patient advocacy, bill reconciliation, and recommendations of quality providers
- Telemedicine-(A strong and growing solution) leading telehealth services aimed at improving patient access and providing convenient quality care
- Clinically Proven Stress Reduction Programs-Solutions to provide individuals with the training to regulate emotional responses and harness the power of heart/brain communication to reduce stress
- Worksite Challenge Programs-Solutions to provide employees with ongoing education and resources to promote development of healthy behaviors
VBA Vision
- Four (4) standard vision plans
- Rates are guaranteed (no underwriting)
- Available to employers with 2 to 24 employees
- Can be offered as non-contributory (100% employer paid) or contributory (any portion paid by the employee)
- Minimum of two (2) employees must be enrolled
- Coverage is effective the 1st of the month following the company’s established new hire waiting period
- Member terminations always effective the last day of the month
- Annual open enrollment is aligned with the employer’s medical plan open enrollment period
- Simplified employer group application
COBRA
The Federal Consolidated Omnibus Budget Reconciliation Act (COBRA) give workers and their families the right to continue group health insurance after the active employee coverage has been terminated due to one of the following qualifying events:
-
- Voluntary or involuntary job loss
- Reduction in hours worked
- Transition between employment
- Death of a loved one
- Divorce or separation
- Spousal loss of benefits
Federal COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50% of its typical business days in the previous calendar year. Both full-and part-time employees are counted to determine whether the plan is subject to COBRA. Each part-time employee counts as a fraction of a full-time employee, with the fraction equal to the number of hours worked divided by the hours an employee must work to be considered full time.
Pennsylvania State Mini-COBRA extends health care options to workers and their families whose coverage was terminated for one of the following qualifying events:
-
- Death of the covered employee
- Termination of employment (voluntary or involuntary) (but not for the employee’s gross misconduct
- Reduction in hours
- Divorce or legal separation
- Eligibility for Medicare
- Dependent child ceasing to be a dependent
Pennsylvania State Mini-COBRA generally applies to all private-sector group health plans maintained by employers that have 19 or less employees.
If you are a PA health care broker and would like to know how you can partner with us,
call 717-591-8280 or contact us here.